New Jersey Department of Health COVID-19 Public Health Recommendations for Reopening Childcare
Effective June 15, 2020, pursuant to Executive Order No. 149 and Executive Directive no. 20-032 all child care programs operating in the State of New Jersey must comply with the requirements detailed in Guidance for New Jersey Child Care Facilities On COVID-19 Related Health and Safety Requirements set forth by the New Jersey Department of Children and Families (DCF). This guidance document outlines COVID-19 public health recommendations for the childcare setting. As this situation is evolving, these recommendations are subject to change as more information is learned about this novel virus. Please check the NJDOH COVID-19 Information for Schools webpage frequently for updated guidance.
Reopening childcare requires everyone to move forward together by practicing social distancing, wearing masks, and performing everyday preventive actions to reduce the spread of respiratory illness. Everyone also has a role in making sure our communities are as safe as possible to reopen and remain open.
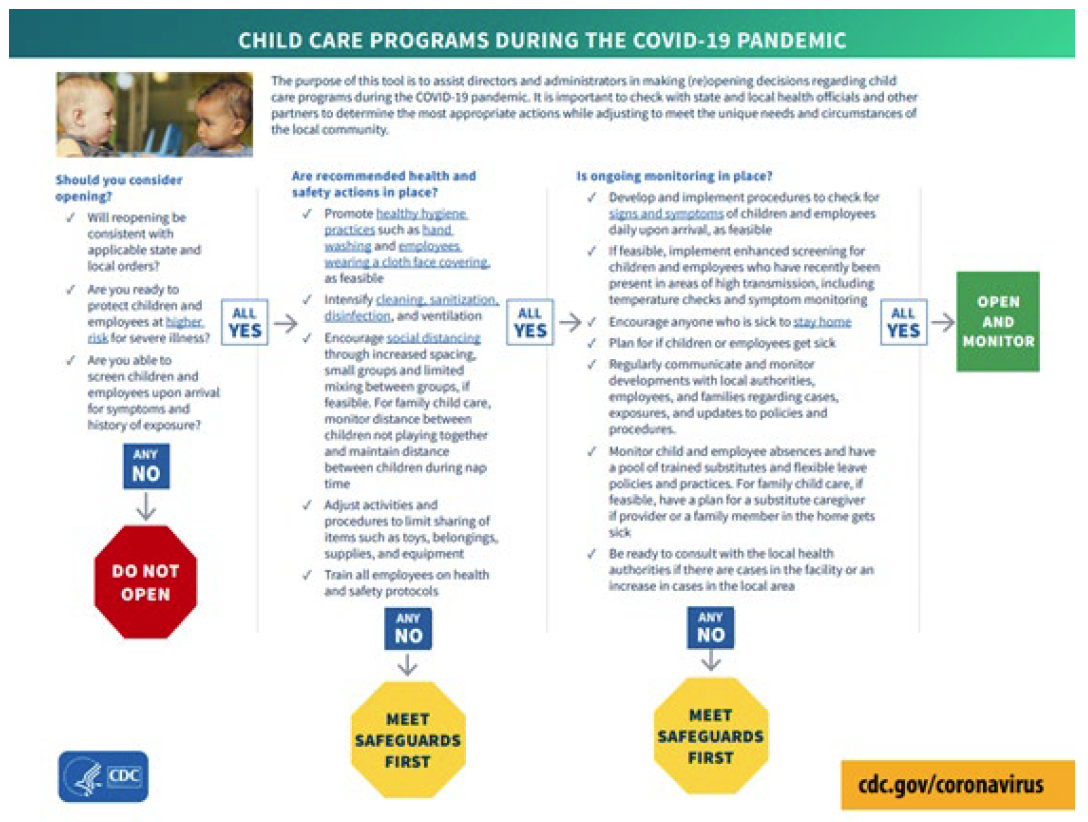
As centers resume operations, they should consider how best to structure services to minimize risk to staff and children in line with the DCF guidelines. CDC’s School and Child Care Programs page provides various resources for recommendations for operating childcare programs in low, moderate, and significant mitigation communities. CDC’s Considerations for Schools have been developed to supplement, not replace, any state or local health and safety laws, rules, and regulations with which childcare centers must comply.
Communication
Childcare centers should develop a plan for infectious disease outbreaks including COVID-19. Staff and families should be informed of policies for ill staff and children including isolation, exclusion and notification of positive cases or outbreaks.
Families should understand what actions they need to take should their child become symptomatic or be exposed to COVID-19 while in childcare.
Designate a staff member to be responsible for responding to COVID-19 concerns. Communicate to staff members the process for contacting the designee.
Establish relationships with local public health officials and identify points of contact.
Create a communication system for staff and families for self-reporting of symptoms and notification of exposures and closures.
CDC’s Guiding Principles to Keep in Mind
The more people a student or staff member interacts with, and the longer that interaction, the higher the risk of COVID-19 spread. The risk of COVID-19 spread increases in school settings as follows:
Lowest Risk: Students and teachers engage in virtual-only classes, activities, and events.
More Risk: Small, in-person classes, activities, and events. Groups of students stay together and with the same teacher throughout/across school days and groups do not mix. Students remain at least 6 feet apart and do not share objects (e.g., hybrid virtual and in-person class structures, or staggered/rotated scheduling to accommodate smaller class sizes).
Highest Risk: Full sized, in-person classes, activities, and events. Students are not spaced apart, share classroom materials or supplies, and mix between classes and activities.
Prepare for Reopening
- Review and update or develop your outbreak response/pandemic plan and share withstakeholders before an outbreak occurs.
- Establish procedures to ensure children and staff who become sick at childcare or arrive at the facility sick are sent home as soon as possible.
- Prepare for the potential of school closures or dismissals.
- Create emergency communication plan and maintain up to date contact information for everyone in your communication chain.
- Plan workshops and trainings to educate staff on prevention measures.
- Continue to monitor current information from health officials.
- Continue to ensure that children are up to date on immunizations.
Cleaning and Disinfection
Child care centers should follow standard procedures for routine cleaning and disinfecting with an EPA-registered product for use against SARS-CoV-2. This means at least daily disinfecting surfaces and objects that are touched often, such as desks, countertops, doorknobs, computer keyboards, hands-on learning items, faucet handles, phones and toys. Information on cleaning and disinfecting your facility can be found at https://www.cdc.gov/coronavirus/2019-ncov/community/disinfecting-building-facility.html Increasing the frequency of cleaning when there is an increase in respiratory or other seasonal illnesses is always a recommended prevention and control measure.
- If a sick child has been isolated in your facility, clean and disinfect surfaces in your isolation room or area after the sick child has gone home. More information on cleaning and disinfection can be found in Guidance for Child Care Programs that Remain Open. If a sick child has been isolated in your facility, clean and disinfect surfaces in your isolation room or area after the sick child has gone home.
- If COVID-19 is confirmed in a child or staff member:
- Close off areas used by the person who is sick.
- Open outside doors and windows to increase air circulation in the areas.
- Wait up to 24 hours or as long as possible before you clean or disinfect to allow respiratory droplets to settle before cleaning and disinfecting.
- Clean and disinfect all areas used by the person who is sick, such as offices, bathrooms, and common areas with an EPA-registered product for use against SARS-CoV-2.
- If more than 7 days have passed since the person who is sick visited or used the facility, additional cleaning and disinfection is not necessary. Continue routine cleaning and disinfection.
Symptom Screening
Child care centers are required to follow screening and admittance requirements for children and staff as outlined in the Guidance for New Jersey Child Care Facilities On COVID-19 Related Health and Safety Requirements.
Parents/caregivers should be strongly encouraged to monitor their children for signs of illness every day as they are the front line for assessing illness in their children. Children and staff who are sick should not attend child care. Centers are encouraged to strictly enforce exclusion criteria for both children and staff.
Centers should provide clear and accessible directions to parents/caregivers and staff for reporting symptoms and reasons for absences.
Preparing for Illness
- Daily reports of staff and student attendance should be closely monitored.
- Designate an area or room away from others to isolate individuals who become ill while at the facility.
- Ensure there is enough space for multiple people placed at least 6 feet apart.
- Ensure hygiene supplies are available, including a cloth mask, facial tissues, and alcohol-based hand rub.
- Establish procedures for safely transporting anyone who is sick to their home or to a healthcare facility. If you are calling an ambulance or bringing someone to the hospital, try to call first to alert them that the person may have COVID-19.
Be ready to follow CDC guidance on how to disinfect your building or facility if someone is sick.
COVID-19 Symptoms
While some children and infants have been sick with COVID-19, adults make up most of the known cases to date. Early research suggests that fewer children than adults with COVID-19 get a fever, cough, or shortness of breath. Few children with COVID-19 have had to be hospitalized. However, severe illness has been reported in children, most often in infants less than a year.
Some children have developed multisystem inflammatory syndrome (MIS-C). Currently, information about this syndrome is limited.
According to the CDC, children do not seem to be at higher risk for getting COVID-19. However, some people, including children with special health care needs, may be at higher risk. Those at increased risk include:
- Older adults
- People who have serious chronic medical conditions like:
- Cancer
- Chronic kidney disease
- COPD
- Immunocompromised state from solid organ transplant
- Obesity (body mass index of 30 or higher)
- Serious heart conditions, such as heart failure, coronary artery disease, or cardiomyopathies
- Sickle cell disease
- Type 2 diabetes
Signs and symptoms of COVID-19 in children may be similar to those of common viral respiratory infections or other childhood illnesses. The overlap between COVID-19 symptoms and other common illnesses means that many people with symptoms of COVID-19 may actually be ill with something else. This is even more likely in young children, who typically have multiple viral illnesses each year. It is important for pediatric providers to have an appropriate suspicion of COVID-19, but also to continue to consider and test for other diagnoses.
Individuals with COVID-19 have had a wide range of symptoms reported – ranging from mild to severe illness. There is not a single symptom that is uniquely predictive of a COVID-19 diagnosis. A COVID-19 viral test is needed to confirm if someone has a current infection. Symptoms may appear 2-14 days after exposure to the virus and include the following:
- Fever or chills
- Cough
- Shortness of breath or difficulty breathing
- Fatigue
- Muscle or body aches
- Headache
- New loss of taste or smell
- Sore throat
- Congestion or runny nose
- Nausea or vomiting
- Diarrhea
Exclusion Criteria
Parents should not send children to childcare when sick. Childcare staff should have plans to isolate children with overt symptoms of any infectious disease that develop during the day while at the childcare facility. Any child that develops a single symptom not including cough, shortness of breath, difficulty breathing, or new taste or olfactory disorder should follow the NJDOH School Exclusion List to determine the exclusion timeframe.
Children who meet the following criteria should be promptly isolated and excluded from the facility for at least 10 days from symptom onset, are fever free for 24 hours without fever reducing medication and symptoms have improved OR they have a negative COVID-19 test result.
- At least two of the following symptoms: fever (measure or subjective), chills, rigors (shivers), myalgia (muscle aches), headache, sore throat, nausea or vomiting, diarrhea, fatigue, congestion or runny nose; OR
- At least one of the following symptoms: cough, shortness of breath, difficulty breathing, new olfactory disorder, new taste disorder.
When Illness Occurs
This guidance is based on what is currently known about the transmission and severity of coronavirus disease 2019 (COVID-19). This is an evolving situation and guidance is subject to change. Please check the NJDOH and CDC websites frequently for updates.
Children and staff with fever, cough, or difficulty breathing should be placed away from others and asked to wear a face mask until they can be sent home.
- Whenever possible, cover children’s (age 2 and older) noses and mouths with a mask.
- If a mask is not tolerated by the child, staff should follow social distancing guidelines (6 ft. away).
- Individuals should be sent home and referred to a healthcare provider. Testing for COVID-19 is recommended for persons with COVID-19 symptoms.
- When an individual tests positive for COVID-19, the facility should immediately notify local health officials, staff and families of the COVID-19 case while maintaining confidentiality.
- Centers should be prepared to provide the following information when consulting public health:
- The identity of the person with COVID-19or probable COVID-19(i.e. staff, child in care, household contact);
- The date the person with COVID-19or probable COVID-19 was last in the building;
- The date the person developed symptoms and/or tested positive;
- Types of interactions the person may have had with other persons in the building or in other locations;
- Names, addresses, and telephone numbers for ill person’s close contacts in the school;
- Any other information to assist with the determination of next steps;
- If other persons in the childcare program have developed any symptoms; and
- Any other informationto assist with the determination of next steps.
COVID-19Illness, Exposure and Exclusion:
Exclusion Duration forclose contacts:
CDC released guidance with options to shorten the quarantine time period following exposure to a confirmed positive case.While CDC and NJDOH continueto endorse 14 daysas the preferred quarantine period–and thus the preferred schoolexclusion period–it is recognized that any quarantine shorter than 14 days balances reduced burden against a small possibility of spreading thevirus. Additional information is described in NJDOH quarantine guidance.
The NJDOH COVID-19 ActivityLevel Index Report (CALI)provides information on COVID-19 transmission risk by region and statewide and characterizes risk asVery High (red), High (orange),moderate (yellow), or low (green).
Childcare administratorsshould have a policy that defines the quarantine timeframe for their population(staff,attendees). NJDOH recommendsthatwhen COVID-19 transmission risk isHigh or Very High(orangeor red CALI score),exposed closecontacts quarantine for 14 days.When the COVID-19 transmission risk isModerateor Low (yellowor greenCALI score), the CDC recommended shortenedtimeframes are acceptablealternatives.
In the childcare setting, excluded individuals who are close contacts of staff or attendees with COVID-19compatible symptoms or who tested positive for COVID-19may be considered for a reduced exclusion period based onRegional Risk Levels:
- High/Very High(orange/Red), exposed close contacts should be excluded from school for14days.
- Moderate or Low (yellow or green),exposed close contacts should be excluded from school for10 daysorafter Day 7 if the individual tests negativewith a viral test (molecular-PCR or antigen)between day 5-7 and if nosymptomswere reported during daily monitoring.
Centers serving medically complex or other high-risk individuals should use a 14-day exclusion period for the exclusion of these individuals or those who work closely with them when identified as close contacts throughout all risk levels.
Children and staff who are COVID-19 positive must not return until they have met the criteria for discontinuing home isolation (see table below).
- Individuals with COVID-19 compatible symptoms should be excluded until they have a negative COVID-19 test or have completed the criteria for discontinuing home isolation. Alternate diagnosis should not be accepted for return to childcare/work.
- The other individuals of the small group/cohort of the symptomatic person should also be sent home. These contacts should be excluded and may return:
- If the ill person tests positive – after the exclusion criteria for a close contact has been met and no symptoms have developed.
- After the ill person tests negative.
|
Individuals who: |
Should stay home and away from others until: |
|
Have symptoms of COVID-19 AND
|
|
|
Have NO symptoms and have tested positive |
|
|
Have symptoms and have tested negative |
|
|
Are identified as a close contact of a case |
|
- If a case of COVID-19 infection occurs in one defined group (see note) within the center, the ill person should be sent home.
- Other staff and children in the group would be considered close contacts of that case and should be excluded and instructed to quarantine in their homes until the exclusion criteria for a close contact has been met.
- Public health, parents/guardians, and staff facility-wide should be informed of the situation.
- The CDC guidance for cleaning and disinfection should be followed.
- Other groups within the childcare facility can continue to function, with daily and vigilant screening for illness occurring, and social distancing, personal and environmental hygiene measures strictly adhered to.
- If cases occur in multiple groups within the facility, then all childcare operations within the facility need to be suspended (see Closure section).
- The ability to keep groups small and static can be helpful in identifying close contacts and may aid in determining if a facility wide closure is necessary.
Note: Per DCF requirements, classes shall include the same group of children each day, to the greatest extent possible, and, also to the greatest extent possible, the same staff shall be assigned to care for each group, each day.
Outbreaks
An outbreak in school settings is defined as two or more laboratory-confirmed COVID-19 cases among students or staff with onsets within a 14-day period, who are epidemiologically linkedclose contacts of each other in another setting during standard case investigation or contact tracing. 1, do not share a household, and were not identified as
Contact Tracing
Childcare staff should help in identifying close contacts of positive COVID-19 cases. This should be done in conjunction with the LHD.
Contact tracing is a strategy used to determine the source of an infection and how it is spreading. Finding people who are close contacts to a person who has tested positive for COVID-19, and therefore at higher risk of becoming infected themselves, can help prevent further spread of the virus.
Close contact is defined as being within 6 feet of someone with suspected or known COVID-19 for 15 or more minutes during a 24-hour period. In some school situations, it may be difficult to determine whether individuals have met this criterion and an entire cohort, classroom, or other group may need to be considered exposed, particularly if people have spent time together indoors.
1 Health departments should verify to the best extent possible that cases were present in the same setting during the same time period (e.g., same classroom, school event, school-based extracurricular activity, school transportation) within 14 days prior to onset date (if symptomatic) or specimen collection date for the first specimen that tested positive (if asymptomatic or onset date is unknown) and that there is no other more likely source of exposure (e.g., household or close contact to a confirmed case outside of educational setting).
A contact tracing team from the local health department or the NJDOH calls anyone who has tested positive for COVID-19. They ask the patient questions about their activities within a certain timeframe, to help identify anyone they have had close contact. Those contacts might include family members, caregivers, co-workers or health care providers.
Individuals who have recently had a close contact with a person with COVID-19 should stay home and monitor their health.
Closure
- A center may need to temporarily dismiss children and staff for 2-5 days, if a child or staff member attended childcare before being confirmed as having COVID-19.
- This initial short-term dismissal allows time for the local health officials to gain a better understanding of the COVID-19 situation impacting the facility, perform contact tracing and cleaning and disinfecting the facility.
- Centers should follow CDC guidance on how to clean and disinfect your building if someone is sick.
- Centers should work with the local health officials to determine appropriate next steps, including whether an extended dismissal duration is needed to stop or slow further spread of COVID-19.
Testing
NJDOH recommends that facilities work with their local health departments to identify rapid viral testing options in their community for the testing of symptomatic individuals. CDC has information on types of COVID-19 tests currently available to diagnose current infection. Having access to rapid COVID-19 testing for ill children and staff can reduce unnecessary exclusion of ill persons and their contacts and minimize unnecessary disruptions of childcare and the educational process.
Until more evidence about protective immunity is available, serologic test results should not be used to make decisions:
- Regarding the need for personal protective equipment.
- To discontinue social distancing measures.
- About grouping persons residing in or being admitted to congregate settings, such as childcare, schools, dormitories, or correctional facilities.
- About returning persons to the workplace.
COVID-19 Resources
NJDCF COVID-19 Resources for Licensed Childcare Centers
CDC Childcare Schools and Youth Programs
CDC Considerations for Youth Sports
NJDOH COVID Information for Schools
CDC Cleaning and Disinfecting Your Facility
CDC Information on Cleaning School Buses
AAP Guidance Related to Childcare During COVID-19
NJDOH General Guidelines for the Prevention and Control of Outbreaks in School Settings
Latest News
- ECEA Lauds State Plan to Align Preschool and Child Care Facilities; Strengthening Mixed Delivery in NJ
- Expansion of Public Preschool in New Jersey: A Presentation to the ECEA and ECEC
- Too many obstacles to private pre-K in state program, providers complain
- Governor Murphy Announces New Proposals to Expand Access to Early Childhood Education and Support Working Families
ECEA Board Officers
President
Gigi Schweikert
Vice President
Lauren Standfast
Secretary
Amy Ragsdale
Treasurer
Fred Ferraro
President Emeritus
Guy Falzarano
Executive Director
Jonathan Jaffe
WRITE ECEA
ECEA
Attn: Jonathan Jaffe
312 North Avenue East
Suite 5
Cranford, NJ 07016
Contact the ECEA Executive Team Here
Early Childhood Education Advocates
312 North Avenue East, Suite 5
Cranford, NJ 07016
c/o Jaffe Communications, Inc.
908-789-0700